Understanding Peritoneal Dialysis: A Comprehensive Guide for Nurses
Peritoneal dialysis (PD) is a life-sustaining treatment for patients with end-stage renal disease (ESRD). As a nurse, it's essential to understand the principles, benefits, and challenges of PD to provide high-quality care to your patients. In this article, we'll delve into the world of peritoneal dialysis, exploring its history, types, benefits, and nursing implications.
History of Peritoneal Dialysis
Peritoneal dialysis has been around for over six decades. The first PD treatment was performed in the 1940s by Dr. G. Ganter, a Swedish physician. Initially, PD was used as a temporary measure for acute kidney injury, but it eventually evolved into a long-term treatment for ESRD. Today, PD is a popular choice for patients with ESRD, offering a flexible and autonomous treatment option.

Types of Peritoneal Dialysis
There are two main types of peritoneal dialysis: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
Continuous Ambulatory Peritoneal Dialysis (CAPD)
CAPD involves manually exchanging dialysis fluid throughout the day. Patients use a catheter to fill their peritoneal cavity with dialysis solution, which is then drained and replaced with fresh solution. CAPD is a flexible treatment option, allowing patients to perform exchanges at home or on-the-go.
Automated Peritoneal Dialysis (APD)
APD uses a machine to perform exchanges during the night while the patient sleeps. APD is also known as Continuous Cycling Peritoneal Dialysis (CCPD). This type of PD is ideal for patients who prefer a more automated treatment option.

Benefits of Peritoneal Dialysis
Peritoneal dialysis offers several benefits for patients with ESRD. Some of the advantages include:
- Flexibility: PD can be performed at home, allowing patients to maintain their independence and lifestyle.
- Autonomy: Patients can manage their treatment schedule and perform exchanges at their convenience.
- Portability: PD is a portable treatment option, making it ideal for patients who travel or have active lifestyles.
- Gentle on the body: PD is a gentle treatment option compared to hemodialysis, which can be stressful on the body.

Nursing Implications
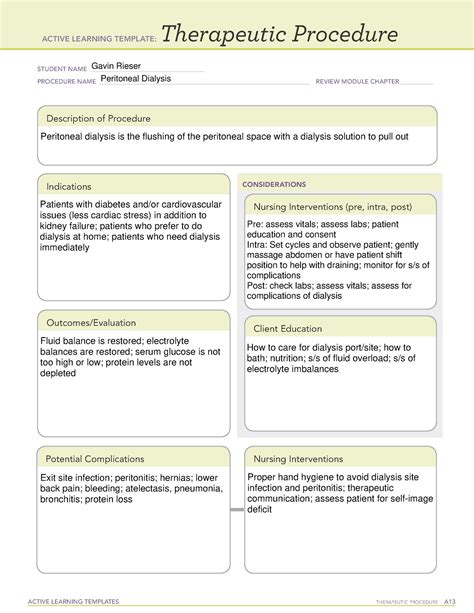
As a nurse, it's essential to understand the nursing implications of peritoneal dialysis. Some of the key implications include:
- Patient education: Educating patients on proper exchange techniques, catheter care, and infection prevention is crucial.
- Catheter care: Nurses must ensure proper catheter care to prevent infection and complications.
- Exchange technique: Nurses should be familiar with exchange techniques to assist patients with manual exchanges.
- Complication management: Nurses should be aware of potential complications, such as peritonitis, and know how to manage them.

Gallery of Peritoneal Dialysis





FAQs
What is peritoneal dialysis?
+Peritoneal dialysis is a treatment for end-stage renal disease (ESRD) that uses the peritoneum, a thin layer of tissue in the abdominal cavity, to filter waste products from the blood.
What are the benefits of peritoneal dialysis?
+Peritoneal dialysis offers several benefits, including flexibility, autonomy, portability, and gentleness on the body.
What are the types of peritoneal dialysis?
+There are two main types of peritoneal dialysis: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
In conclusion, peritoneal dialysis is a valuable treatment option for patients with end-stage renal disease. As a nurse, it's essential to understand the principles, benefits, and nursing implications of PD to provide high-quality care to your patients. By educating yourself on PD, you can help patients manage their treatment and improve their quality of life.